Children, Influencers, and Impulse Buying Online
You may have seen news outlets reporting on the trend...

TeacherLists Surpasses One Million School Supply Lists on its Platform
FOR IMMEDIATE RELEASE
PRESS RELEASE
TeacherLists
100...

What Teachers Want You to Know About Back-to-School
Teachers have a difficult job, and one that doesn’t...

Books, Movies, and TV Shows to Binge: Parent Recommendations
Are you a book worm, or do you prefer watching...

How to Talk to your Child About Their World
Help your child feel safe while staying informed with...
Tips and Tricks for a Successful Back-to-School Routine
Back-to-school season is in full swing! Whether your...
No Image found
8 Books for Overcoming Back-to-School Anxiety
Many kids feel a whirlwind of emotions before the new school...

What is the Metaverse—and should you be concerned?
What do you call an all-encompassing online world your...

10 Ways to Honor Memorial Day with your Children
Check out these tips to honor Memorial Day, shared...

Mother’s Day “Mom-Me” Time Activities from Real Moms
Me time activities from real moms, just in time for Mother’s...

Teacher Appreciation Week: The Do’s and Don’ts
Check out these tips for how to, and how not to, thank...

Standardized Tests: Tips and Tricks to Prepare Your Children
Ease test anxiety with these tips and tricks!

5 Tips to Promote Social-Emotional Development at Home
Social-emotional development is fundamental for success....
Screen Time: the good, the bad, and the balance
Unlock the benefits to screen time. The key is striking...
The 10 Most Boring (But Awesome!) Gifts for Teachers
Believe it or not, teachers love receiving school supplies...
Set Kids Up for School Success: Healthy Habits Parents Can Teach Their Kids
By establishing important eating, sleeping, and learning...
7 Smart Tips To Help You Ace Back-to-School Shopping
On paper, the idea of back-to-school shopping is exciting...
Shop Your Supply Lists During Tax-Free Weekends
Take advantage of the back-to-school timing of states'...

Talking to Kids About Anti-Racism and Race Relations
Conversations with kids about race relations can be hard,...

Science for Kids: 28+ STEM Activities To Do at Home
Step-by-step instructions and materials lists for family-friendly...
Parents: You Should Know This Internet Slang
There's a good chance a lot more kids will be spending...
After-School Snacks: Healthy Options for Kids
Fun ideas for healthy after-school snacks kids will...
Understanding Report Cards: A Guide for Parents
Letter grades are being replaced by number systems...

Learning Styles Quiz: What Is Your Child's Learning Style?
Understanding how your child learns can reduce frustration...
Helping Students Adjust to the New School Year: Teacher Tips for Parents
Back-to-school tips for families
School Success - 10 Ways Parents Can Help: Teacher Tips for Parents
School Success—10 Ways Parents Can Help
Teachers...

10 Ways To Help Kids Handle Back-to-School Anxiety: Teacher Tips for Parents
10 Ways To Help Kids Handle Back-to-School Anxiety:...

Make Parents Your Partner: Teacher Tips for Parents
Teachers: Make Parents Your Partner
Building strong...

Homework Tips for Parents: Teacher Tips for Parents
Homework Tips for Parents
When the last bell rings...
No Image found
Student Goal Setting: 3 Teacher Tips for Parents
Student Goal Setting: 3 Steps to Success
January is a great...

At-Home Learning Tips for Parents: Teacher Tips for Parents
At-Home Learning Tips for Parents
While teachers play...

Guide to Parent-Teacher Conferences: Teacher Tips for Parents
Why Attend a Parent-Teacher Conference?
Parent-teacher...
No Image found
The Top Teacher Gifts You Can Find on Amazon Right Now
The top gifts for teachers this holiday season. Apparel,...
No Image found
Black Friday Deals for Everyone on Your List
Kittaya Mangruan/123RF
Whether you’ll be getting...
No Image found
How to Use One-Click Shopping Right From Your List
You've found your child's supply list and now you want...
No Image found
How Parent Groups can help their Schools with TeacherLists
Are you a Parent or part of a Parent Group (PTO/PTA/PTSO/HSA,...
No Image found
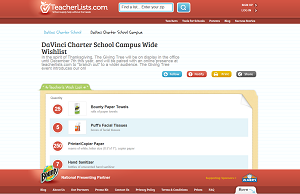
How To Use Amazon To Purchase TeacherLists Wish List Items
Step-by-step instructions to make donating classroom...
No Image found
What You Need to Know About Back-to-School Shopping In Your State
There are so many funny blogs out there about what...
No Image found
How To Find Your School's Supply Lists on TeacherLists
Find your child’s school supply lists and classroom...